Borderline personality disorder (BPD) and autism spectrum disorder (ASD) are both complex neurodevelopmental conditions that can coexist in some individuals, leading to unique challenges in diagnosis and treatment.
Understanding the comorbidity of these two disorders requires exploring their distinct features, overlaps, diagnostic criteria, and potential implications for management and support.

Borderline Personality Disorder (BPD)
Borderline personality disorder is characterized by pervasive instability in mood, interpersonal relationships, self-image, and behavior. Individuals with BPD often experience intense emotional turmoil, impulsivity, fear of abandonment, and a chronic sense of emptiness. These symptoms can significantly impair daily functioning and quality of life.
BPD affects approximately 1-2% of the general population in the US and is more common among women than men.
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), the primary diagnostic criteria for BPD include:
- Frantic efforts to avoid real or imagined abandonment.
- A pattern of unstable and intense interpersonal relationships.
- Identity disturbance: markedly and persistently unstable self-image or sense of self.
- Impulsivity in at least two areas that are potentially self-damaging (e.g., spending, sex, substance abuse, reckless driving).
- Recurrent suicidal behavior, gestures, threats, or self-mutilating behavior.
- Affective instability due to a marked reactivity of mood (e.g., intense episodic dysphoria, irritability, or anxiety usually lasting a few hours and only rarely more than a few days).
- Chronic feelings of emptiness.
- Inappropriate, intense anger or difficulty controlling anger (e.g., frequent displays of temper, constant anger, recurrent physical fights).
- Transient, stress-related paranoid ideation or severe dissociative symptoms.
Autism Spectrum Disorder (ASD)
On the other hand, autism spectrum disorder is a developmental disorder characterized by difficulties in social interaction and communication, alongside restricted and repetitive patterns of behavior, interests, or activities. ASD encompasses a wide range of symptoms, skills, and levels of impairment, from mild to severe.
It affects about 1 in 54 children in the United States, with boys being four times more likely than girls to be diagnosed.
The DSM-5 outlines the diagnostic criteria for autism spectrum disorder, which include:
- Persistent deficits in social communication and social interaction across multiple contexts.
- Restricted, repetitive patterns of behavior, interests, or activities.
- Symptoms must be present in early childhood, even if they may not become fully manifest until social demands exceed limited capacities.
- Symptoms cause clinically significant impairment in social, occupational, or other important areas of current functioning.
Comorbidity of BPD and ASD
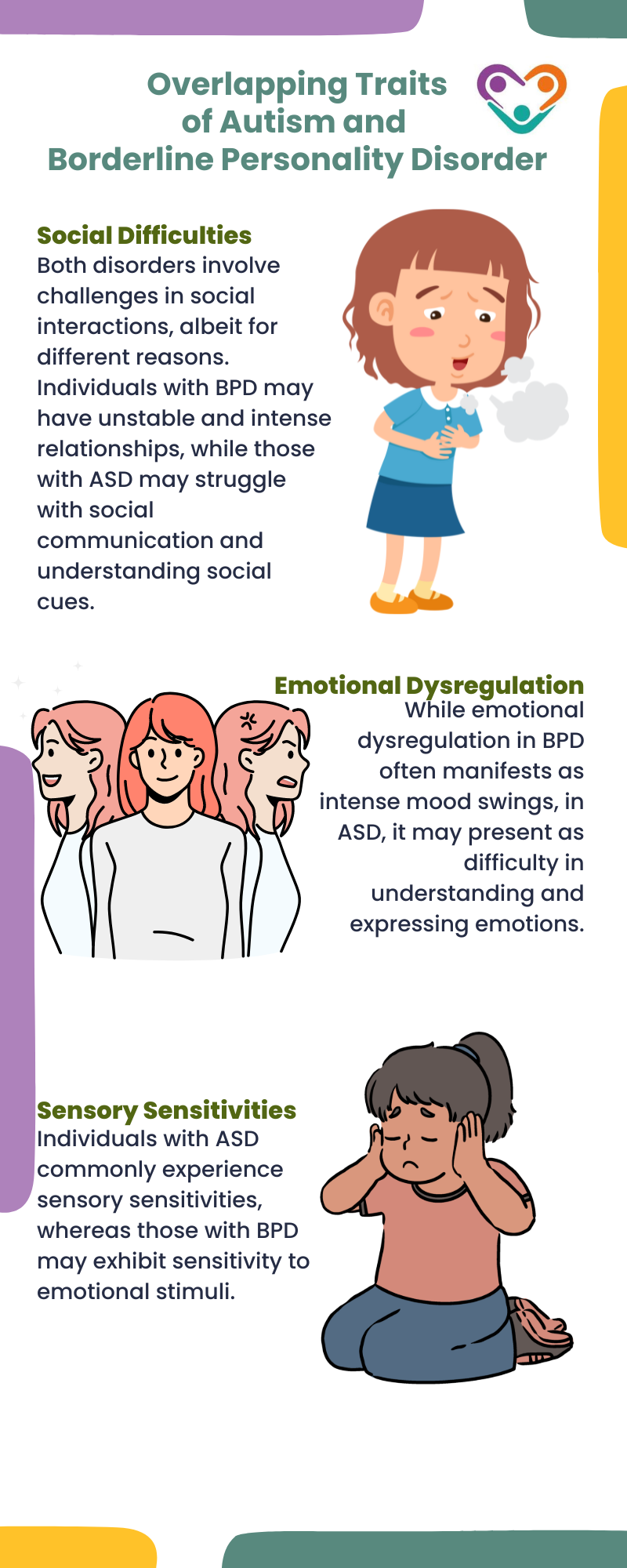
Research suggests that BPD and ASD can co-occur more frequently than would be expected by chance alone. While they are distinct conditions with different core features, some overlapping traits can complicate diagnosis and treatment.
For instance, individuals with both BPD and ASD may exhibit:
Challenges in Diagnosis and Treatment
Diagnosing BPD and ASD together can be challenging due to their overlapping symptoms and the tendency for symptoms to present differently in each individual. Clinicians must carefully evaluate the full range of symptoms and their developmental history to make accurate diagnoses.
Treatment for individuals with comorbid BPD and ASD often requires a multidisciplinary approach that addresses both conditions simultaneously. This may include the following:
- Psychotherapy – Dialectical Behavior Therapy (DBT) has shown effectiveness in treating BPD, focusing on emotion regulation, interpersonal effectiveness, distress tolerance, and mindfulness. Modified versions of DBT or other therapies tailored to accommodate the cognitive and social deficits of ASD may be beneficial.
- Medication – Psychiatric medications may be prescribed to manage specific symptoms such as mood instability or anxiety, although their efficacy in individuals with comorbid BPD and ASD requires careful consideration.
- Supportive interventions – Social skills training, occupational therapy, and educational supports can help individuals with ASD navigate social interactions and daily activities, while also addressing the emotional dysregulation characteristic of BPD.
Research and Future Directions
While there is growing recognition of the overlap between BPD and ASD, further research is needed to elucidate the underlying mechanisms and optimal treatment strategies for individuals with both conditions.
Longitudinal studies examining the developmental trajectories of these disorders and large-scale clinical trials evaluating integrated treatment approaches are crucial for improving outcomes and quality of life for affected individuals.
Borderline personality disorder and autism spectrum disorder can coexist in some individuals, posing diagnostic and therapeutic challenges due to their overlapping symptoms and distinct clinical presentations. Understanding the comorbidity of these disorders requires a nuanced approach that acknowledges both the similarities and differences in their symptomatology and treatment needs.
By integrating insights from clinical research and adopting tailored therapeutic interventions, clinicians can better support individuals with comorbid BPD and ASD in achieving improved functional outcomes and overall well-being.
Sources:





